Understanding Metabolic factors & MSK Pain
Thanks for reading the 12th edition of my newsletter. This newsletter tracks my work to create the best available resource for newly qualified physiotherapists interested in MSK.
Lately, I’ve noticed more and more patients coming in with one or two metabolic conditions—things like obesity or metabolic syndrome. And guess what? They’re also dealing with osteoarthritis, tendon pain, and low back pain. It made me wonder if there’s a real connection between the two. What’s the actual pathophysiology behind it all, beyond just low-grade inflammation?
In this episode, I’ll dive into it:
Explore the common inflammatory pathways activated in obesity and metabolic syndrome.
Discuss how they contribute to musculoskeletal disorders.
Suggest potential treatment strategies for physiotherapists working with these patients.
Obesity and metabolic syndrome aren’t just public health buzzwords—they’re serious conditions that impact everything from cardiovascular health to, as we’ll see, your joints and muscles. What’s really interesting is how they’re linked to chronic, low-grade inflammation, which seems to drive a lot of the musculoskeletal issues we see. If you’re a physiotherapist like me, getting a handle on this inflammation is key to helping your patients.
Understanding Obesity and Metabolic Syndrome
Before we get into the nitty-gritty of inflammation, let’s recap what these terms actually mean.
Obesity: We’re talking about excess fat that poses a health risk, usually when someone’s body mass index (BMI) hits 30 or higher.
Metabolic syndrome: It’s a cluster of conditions (insulin resistance, hypertension, hyperlipidemia, and central obesity) that increase the risk of heart disease and type 2 diabetes.
Both are closely linked to inflammation, which can wreak havoc on the body—including the musculoskeletal system.
Chronic Low-Grade Inflammation in Obesity and Metabolic Syndrome
So, what’s actually happening with the inflammation here? It’s not just a mild annoyance; it’s a complex process that affects a lot of body systems, including the muscles and joints.
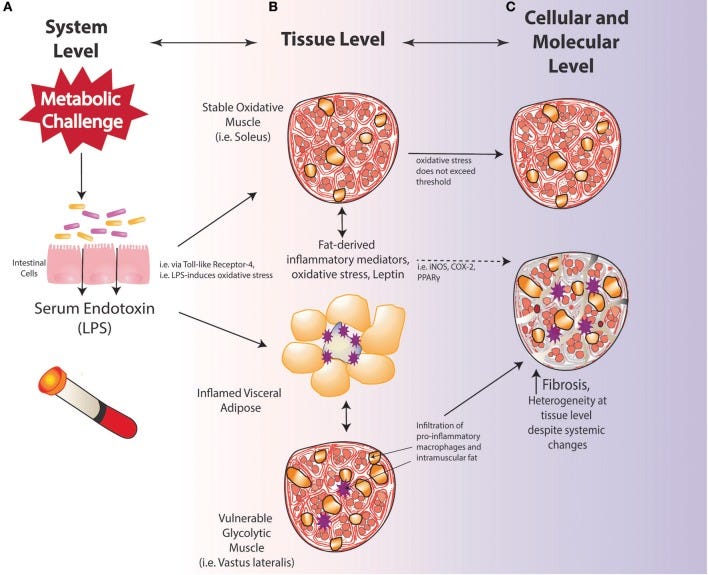
.1. Adipose Tissue: More Than Fat Storage
Turns out, fat isn’t just sitting there, storing energy. It’s an active endocrine organ that releases all sorts of signaling molecules, called adipokines, like leptin and adiponectin—plus some heavy-hitting pro-inflammatory ones like TNF-α and IL-6. In obesity, this secretion gets out of whack, driving widespread inflammation.
.2. Pro-Inflammatory Cytokines: The Usual Suspects
When we think about inflammation in obesity, the main culprits are cytokines like:
TNF-α: Released by macrophages, this one not only plays a role in insulin resistance but also kicks off other inflammatory responses through NF-κB activation.
IL-6: Elevated in obesity, it boosts C-reactive protein (CRP) levels and contributes to the whole inflammatory cascade.
IL-1β: This one amplifies the inflammation even more, keeping the cycle going.
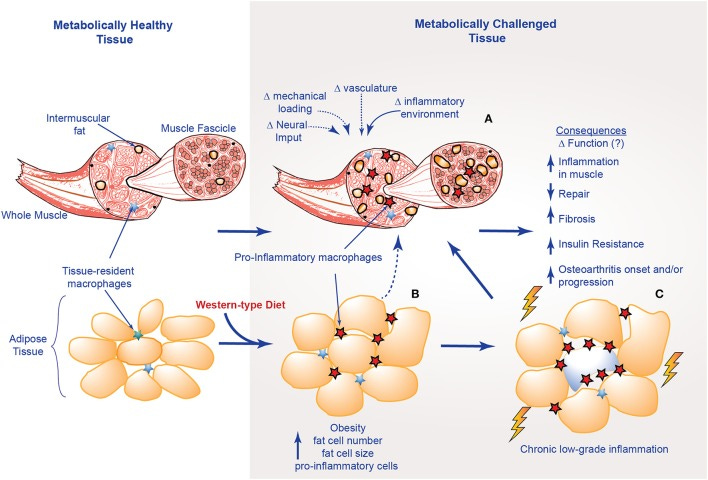
.3. Immune Cells and Their Role
In obesity, immune cells like macrophages infiltrate fat tissue. In lean folks, these macrophages are anti-inflammatory, but in obesity, they switch to a more aggressive, pro-inflammatory type. These M1 macrophages are basically tiny factories pumping out inflammatory cytokines.
.4. Inflammasome Activation and Oxidative Stress
Metabolic syndrome cranks up the inflammasome machinery, particularly the NLRP3 inflammasome, thanks to high blood sugar, free fatty acids, and oxidative stress. This just keeps feeding the fire of inflammation.
Plus, oxidative stress from too many free radicals and dysfunctional mitochondria only makes things worse by activating even more inflammatory pathways, like NF-κB.
Inflammation’s Impact on the Musculoskeletal System
Chronic low-grade inflammation associated with obesity and metabolic syndrome affects the musculoskeletal system in multiple ways, contributing to conditions such as osteoarthritis (OA), sarcopenia, tendinopathy, and chronic low back pain. Here are the key inflammatory mechanisms involved:
.1. Osteoarthritis
OA is one of the most common musculoskeletal conditions associated with obesity. Although traditionally thought to be a purely mechanical condition due to excess weight, inflammation plays a critical role in its development.
Inflammatory Cytokines: Pro-inflammatory cytokines like TNF-α and IL-6 are elevated in the synovial fluid of patients with OA. These cytokines promote cartilage degradation by upregulating matrix metalloproteinases (MMPs), enzymes that break down the extracellular matrix of the cartilage.
Leptin: This adipokine is elevated in obesity and has been found in synovial fluid, where it promotes the production of inflammatory mediators and contributes to cartilage destruction.
Adipose Tissue Infiltration: Obesity leads to increased fat accumulation in joints, such as the infrapatellar fat pad (Hoffa's fat pad), which secretes inflammatory mediators that exacerbate local joint inflammation and cartilage damage.
.2. Sarcopenia
Sarcopenia, the progressive loss of skeletal muscle mass and function, is exacerbated by obesity and metabolic syndrome, a condition known as "sarcopenic obesity."
Chronic Inflammation: Pro-inflammatory cytokines, particularly IL-6 and TNF-α, are involved in the muscle wasting process. TNF-α inhibits the anabolic signaling pathway of insulin-like growth factor 1 (IGF-1), which is crucial for muscle protein synthesis. Additionally, IL-6 promotes muscle breakdown by activating the ubiquitin-proteasome pathway.
Oxidative Stress: Obesity-related oxidative stress contributes to mitochondrial dysfunction in muscle cells, further accelerating muscle degradation and impairing muscle regeneration.
Insulin Resistance: A hallmark of metabolic syndrome, insulin resistance impairs glucose uptake in skeletal muscle, leading to muscle atrophy and a loss of muscle strength.
.3. Tendinopathy
Tendinopathy, a common overuse injury affecting tendons, is more prevalent in obese individuals, partly due to inflammation.
Adipokines and Tendon Degeneration: Adipokines such as leptin and adiponectin have been shown to influence tendon cell function. Leptin, in particular, promotes the expression of MMPs in tendon cells, leading to collagen breakdown and weakening of the tendon structure.
Inflammatory Cytokines: Elevated levels of TNF-α and IL-6 in obesity may contribute to tendinopathy by promoting the degradation of tendon extracellular matrix and impairing tendon healing processes.
.4. Chronic Low Back Pain
Chronic low back pain is another musculoskeletal disorder frequently associated with obesity and metabolic syndrome.
Systemic Inflammation: The low-grade systemic inflammation seen in obesity may contribute to CLBP by sensitizing pain receptors and promoting neuroinflammation in spinal structures.
Disc Degeneration: Obesity is linked to intervertebral disc degeneration, possibly through increased mechanical loading and the pro-inflammatory effects of adipokines like leptin, which promotes the production of degradative enzymes in the intervertebral disc.
Muscle Dysfunction: Sarcopenia and insulin resistance can impair the function of the muscles supporting the spine, leading to altered biomechanics and an increased risk of injury and pain.
So, there you have it—a quick tour through the link between metabolic conditions and musculoskeletal disorders, and why inflammation is the key player. Hopefully, this helps you get a better sense of what’s going on beneath the surface and gives you some ideas on how to approach treatment.
Catch you next time!
Justin
Reference
Abate, M. (2014). How obesity modifies tendons (implications for athletic activities). Muscles, Ligaments and Tendons Journal, 4(3), 298–302.
Abate, M., Salini, V., & Andia, I. (2016). How Obesity Affects Tendons? Advances in Experimental Medicine and Biology, 920, 167–177. https://doi.org/10.1007/978-3-319-33943-6_15
Abate, M., Schiavone, C., Salini, V., & Andia, I. (2013). Occurrence of tendon pathologies in metabolic disorders. Rheumatology, 52(3), 599–608. https://doi.org/10.1093/rheumatology/kes395
Dean, B. J. F., Getgood, A., & Carr, A. J. (2018). The Burden of Tendinopathy in the Workforce. The Journal of Bone and Joint Surgery. American Volume, 100(7), 600–607.