In your initial appointment clinic today, you have a 50-year-old female with 4 month history of R shoulder pain after moving her house. She is pre-diabetic and she is very anxious about her pain, she is also very adamant about having a firm diagnosis.
On examination, she has reduced active range of movement in both flexion and abduction and reports a painful arc. She also reports reduced external rotation and internal rotation in both active and passive ranges. You couldn’t be sure if it is limited by her extreme pain or stiffness.
After your examination, you came up with a few provisional diagnoses
Rotator cuff-related shoulder pain
Frozen shoulder
Degen Rotator cuff tear
Each of them has its own supporting symptoms from the patient’s profile and examination findings.
You are not sure what the diagnosis is. The patient wants a diagnosis today. You have 10 minutes left.
Do you know what to do?
I certainly don’t at that time when I first qualified. I was feeling anxious because I wasn’t sure how to give an exact diagnosis. I wanted to be confident in front of a patient because they are in a lot of pain; I also need to make their 3-month waiting time worthwhile. I was also quite embarrassed because I feel like I wasn’t really providing much help.
After the consultation, I went to find out a bit more about it because I have a feeling that it will not be just me that is facing this scenario.
I eventually came to the phenomenon that resembles the situation
Diagnostic Uncertainty
Looking at the research, diagnostic uncertainty was heavily researched in primary care. What is less talked about, is that students and other novice professionals are also challenged by diagnostic uncertainty. Reasons include the negative emotional reactions to uncertainty, a lack of role models who openly share the uncertainty and a lack of curriculum opportunities during training to experience and manage this dilemma
Hence the purpose of this week’s blog:
Explain what diagnostic uncertainty is
Discuss some of the research
How we (especially newly qualified physios and students) can manage diagnostic uncertainty
Students are often rewarded for displaying confidence and certainty in clinical education settings which may further exacerbate this issue.
Definition of Diagnostic Uncertainty
I asked ChatGPT for some help in defining the term and it came up with
Diagnostic uncertainty has been defined as a subjective perception of an inability to provide an accurate explanation of the patient's health problem
Effects of Diagnostic Uncertainty
Uncertainty has far-reaching effects on patients, clinicians, and health systems.
Mismanagement of diagnostic uncertainty may affect patients by
Decreasing satisfaction, confidence and trust in the medical system c
Causing anxiety and stress
Increasing testing and hospital readmissions
Negatively affecting treatment response (e.g., in chronic pain, uncertainty around overlooking another diagnosis may lessen treatment effects)
Diagnostic uncertainty certainly affects clinicians in ways of
Leading to stress, anxiety, and burnout
Withholding treatments from patients if they assume patients would have negative reactions related to ambiguities in medical tests or the effectiveness of medical treatments
Increased healthcare costs (Further imaging and test)
Uncertainty goes both ways
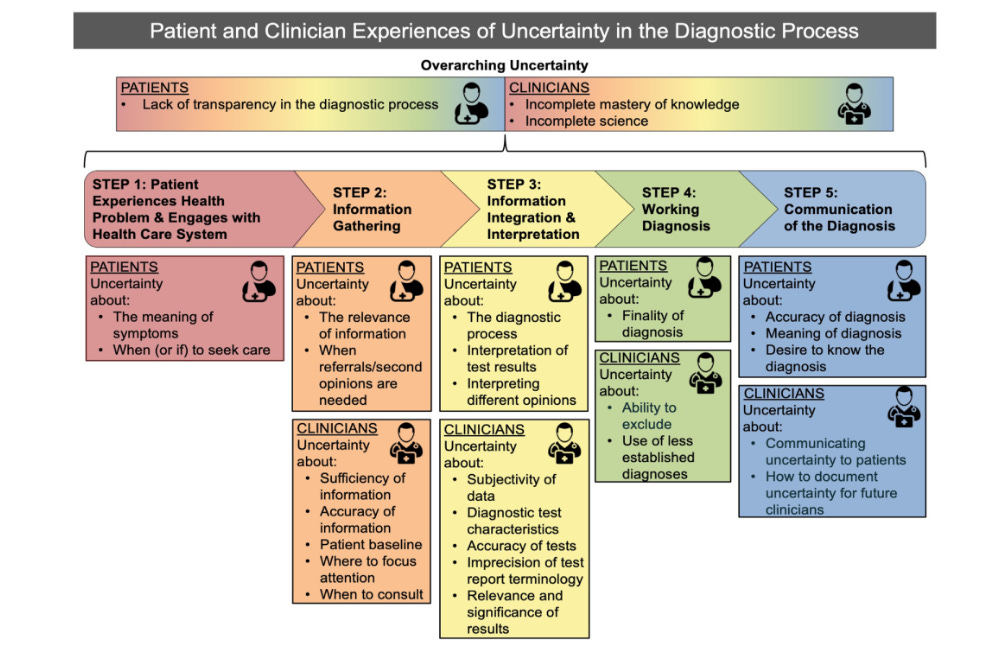
My previous thoughts were that clinicians were the only side that was affected by diagnostic uncertainty. Meyer et al found that at every phase of the healthcare system that will be a risk of uncertainty to BOTH parties
Managing Diagnostic uncertainty
Apart from doing my own research, I have also asked Twitter about their anecdotal experience. I have received a great response to the tweet and have summarised the points below…
Acknowledge uncertainty
We as humans are hardwired to seek certainty and thus we actively avoid unpleasant emotions that arise from uncertainty. Setting the right expectations that it is not something that we can eliminate would be helpful!
Focusing on what matters most to the patients (@LukeTodd)
It can be easy to get hung up on theorising specific diagnoses when a lot of the time patients don’t care if it’s a disc or ligament injury. They just want to improve their pain/function/quality of life. Apart from a solid subjective history of the pain, obtain more contextual knowledge of the patients: find out more about patients’ family situations and their occupations. Ask about their thoughts and feelings about the presenting condition.
Clear red flags and safety netting
Make sure you screen for serious pathologies. If there is none present this can be an important piece of information to reassure the patient. (Most of us would break a sigh of relief when we know there isn’t anything serious!) Inform patients and their families what red flags they should look for after visits, how they should seek additional help if symptoms change or worsen, and what to expect regarding the time course of their symptoms.
Communication
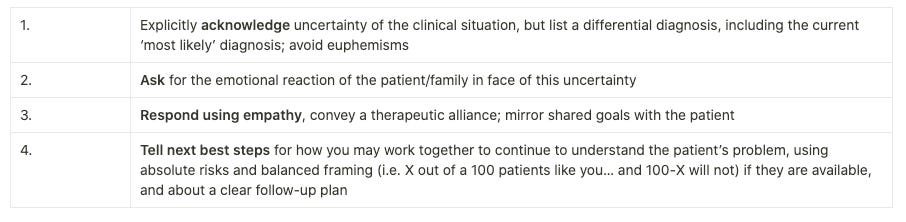
One of the more important skills in managing uncertainty is how we communicate with patients. Some of the principles are being transparent, talking through the findings and reasoning and asking for feedback. Having some form of structure always helps. Below is a model recommended by Santhost et al 2019
A four-step model for communicating with patients about diagnostic uncertainty.
Add-on tip: Normalise the phrase: I am not too sure
I realised that back then I was afraid to show incompetence to the patient. I was quite surprised that research found that physicians’ expressions of uncertainty (‘I don’t know…’), although uncommon, were not associated with lower patient ratings of the physician. Hence it is important to be transparent. Normalise “I don’t know” or “I am not sure” AND discuss your next plan eg: Checking with the senior. It shows strength and not incompetence!
Seek opinions
Few of the answers to my Twitter question revolve around asking for help. As students, we are trained to escalate patients with red flags. Equally, we can escalate and seek opinions EVEN when there isn’t a serious clinical concern. MDT meetings, complex case reviews and peer review sessions can be useful to go through the cases.
Reflection
I personally think reflection is the most important step! Write it out, talk it through. Any output would help with clinical reasoning. Also think about what went well, what didn’t go so well and how we can improve the next time!
There you go, a summary of what is diagnostic uncertainty, why is it important to manage and practical steps to manage it (as per evidence and anecdotal experience from smart people I follow on Twitter) It is also important to acknowledge that it’s common to have uncertainty no matter how experienced you are as a clinician.
The goal is not how to eliminate it but how to manage it.
See you next time
Justin
Resources
So many people quoted so many useful resources. Find them all here!

References
Alam, R. et al. (2017) “Managing diagnostic uncertainty in primary care: A systematic critical review,” BMC Family Practice, 18(1). Available at: https://doi.org/10.1186/s12875-017-0650-0.
Almond, A., Zou, Y. and Forbes, R. (2021) “Navigating diagnostic uncertainty in musculoskeletal practice: The perspectives and experiences of new graduate physiotherapists,” Musculoskeletal Science and Practice, 52, p. 102354. Available at: https://doi.org/10.1016/j.msksp.2021.102354.
Cox, C.L. et al. (2021) “Diagnostic uncertainty in primary care: What is known about its communication, and what are the associated ethical issues?,” Family Practice, 38(5), pp. 654–668. Available at: https://doi.org/10.1093/fampra/cmab023.
Dahm, M.R. and Crock, C. (2022) “Understanding and communicating uncertainty in achieving diagnostic excellence,” JAMA, 327(12), p. 1127. Available at: https://doi.org/10.1001/jama.2022.2141.
Forbes, R. and Toloui-Wallace, J. (2021) “Diagnostic uncertainty in musculoskeletal pain: Implications for physiotherapy education,” OpenPhysio Journal [Preprint]. Available at: https://doi.org/10.14426/opj/a20220202.
Meyer, A.N.D. et al. (2021) “Patient and clinician experiences of uncertainty in the diagnostic process: Current Understanding and Future Directions,” Patient Education and Counseling, 104(11), pp. 2606–2615. Available at: https://doi.org/10.1016/j.pec.2021.07.028.
Santhosh, L., Chou, C.L. and Connor, D.M. (2019) “Diagnostic uncertainty: From education to communication,” Diagnosis, 6(2), pp. 121–126. Available at: https://doi.org/10.1515/dx-2018-0088.

Excellent work mate!
This is very good Justin.